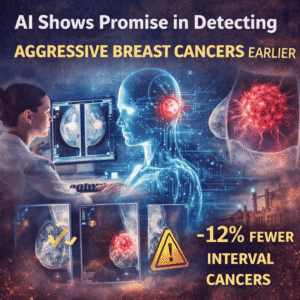
A landmark randomized trial in Sweden offers compelling evidence that AI improves early detection of aggressive breast cancers. Conducted across nearly 100,000 women, the study compared traditional double-reading mammography with AI-supported screening. Results indicate that AI not only boosts detection rates but also helps reduce the number of interval cancers—those that arise and are diagnosed between regular screenings.
Interval cancers are typically more aggressive and difficult to treat. In this study, the AI-assisted group saw 12% fewer interval cancers than the control group. This marks a critical shift in breast cancer screening strategy, as early-stage detection is strongly correlated with improved survival outcomes.
The trial’s protocol involved using an AI system to pre-screen mammograms and highlight high-risk cases. These flagged images were then reviewed by radiologists, making the process a hybrid rather than a fully automated one. This integration meant radiologists could focus on higher-risk scans, optimizing both time and accuracy.
One of the most significant findings was that AI improves early detection of aggressive breast cancers without raising false positives. In fact, the AI-assisted group detected more cancers at the time of screening—81% versus 74% in the traditional reading group—suggesting that AI tools can identify suspicious features that may otherwise escape human review.
Beyond detection, the system improved workflow efficiency. By identifying low-risk scans that required minimal scrutiny, radiologists could devote more attention to complex cases. This is a major advantage, especially in systems struggling with radiologist shortages.
Importantly, the AI did not replace clinicians. It served as a decision-support system, providing risk scores and image annotations to help radiologists make more informed decisions. This model preserves professional judgment while enhancing diagnostic precision—a key consideration in medical ethics and patient safety.
Researchers emphasized that results must be interpreted carefully. The technology’s success depends on factors like the diversity of imaging data, population differences, and infrastructure readiness. AI models trained on limited datasets may underperform when applied to other domains. Global applicability will require local validation and adaptation to different healthcare systems.
Nevertheless, this study is a strong signal that AI, when rigorously tested and responsibly deployed, can be a valuable tool in national breast screening programs. As AI adoption scales, continued monitoring of outcomes, bias mitigation, and public trust will be essential.
In the evolving landscape of oncology diagnostics, the evidence now suggests that AI improves early detection of aggressive breast cancers, creating opportunities to intervene sooner, treat more effectively, and ultimately save lives.